Relevance for UPSC CSE:
- Relevance for Prelims: Key facts, features, number of beneficiaries, treatment packages, funding pattern, empanelled hospitals, Ayushman card coverage, recent expansions to senior citizens and frontline health workers, and digital initiatives such as ABDM.
- Mains: GS Paper-2 – Social Justice – Health: Achievements in improving healthcare access, challenges in implementation, impact on health equity, financial protection, case studies (Haryana), and reforms for better sustainability.
Context / Why in News?
- In August 2025, around 650 private hospitals in Haryana suspended services under AB-PMJAY over pending dues of nearly ₹490 crore.
- The Indian Medical Association (IMA) in Haryana claims payments are delayed despite government assurances, highlighting operational and financial challenges in the scheme’s state-level implementation.

Introduction to AB-PMJAY
- Launched on 23 September 2018, AB-PMJAY is the world’s largest government-funded health assurance programme.
- It provides ₹5 lakh per family per year for secondary and tertiary care hospitalisation to over 12 crore poor and vulnerable families, covering around 55 crore beneficiaries.
- Implemented by the National Health Authority (NHA), the scheme is a core pillar of the government’s Universal Health Coverage strategy and directly supports SDG 3.8 (Universal Health Coverage).
Key Objectives of AB-PMJAY
- Reduce out-of-pocket expenditure (OOPE) on healthcare.
- Improve access to quality and affordable healthcare services for the poor.
- Enhance efficiency and transparency in service delivery.
- Promote preventive, promotive, and curative interventions.
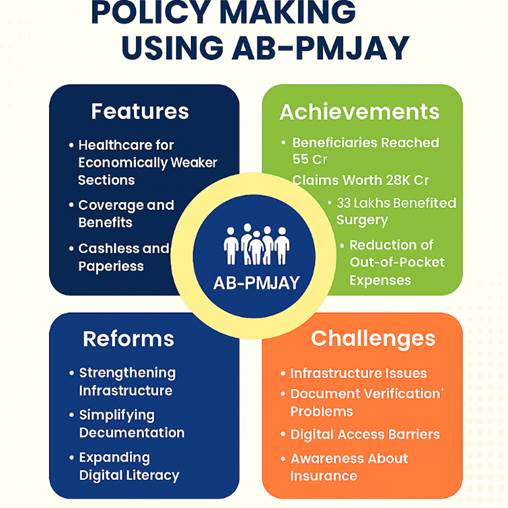
Key Features of AB-PMJAY
- Coverage & Beneficiaries:
- ₹5 lakh health cover per family annually.
- Targets the bottom 40% of the population based on SECC data, now expanded to include senior citizens (70+) and 37 lakh frontline health workers and their families.
- Treatment Packages:
- 1,949 packages covering cancer, cardiac care, orthopaedics, neurosurgery, burns, mental health, etc.
- Standard treatment guidelines ensure uniform quality.
- Funding Pattern:
- Centrally sponsored scheme.
- Funding ratio: 60:40 (Centre:State) for most states, 90:10 for NE/Himalayan states, 100% central funding for UTs without legislature.
- IT & Digital Infrastructure:
- Robust IT platform for beneficiary identification, hospital empanelment, claim processing, and fraud detection.
- Integration with Ayushman Bharat Digital Mission (ABDM) for interoperable health records.
- Hospital Empanelment & PPP Models:
- Over 31,466 empanelled hospitals (14,194 private) as of July 2025.
- Encourages public–private partnerships via trust, insurance, and hybrid models.
- Portability:
- Beneficiaries can access services in any empanelled hospital across India — particularly beneficial for migrants.
- Arogya Mitras:
- Frontline facilitators assisting with registration, pre-authorisation, and claims at hospitals.
- Monitoring & Anti-Fraud Measures:
- National & State Anti-Fraud Units using AI/ML to detect irregularities.
- Over 210 hospitals de-empanelled for malpractice.
Growth and Achievements
- Ayushman Cards Issued: Over 41 crore as of July 2025.
- Admissions & Financial Coverage: More than 9.84 crore admissions authorised; treatments worth ₹1.4 lakh crore funded since launch.
- Financial Protection: OOPE reduced from 62.6% (2015) to 39.4% (2022); GHE increased from 29% to 48% in the same period.
- Savings: Estimated ₹1.25 lakh crore saved for beneficiary households.
- Gender Inclusion: 48% of beneficiaries are women; specific health packages introduced for the transgender community.
- Impact on Care Access: 90% improvement in timely cancer treatment access among beneficiaries.
- Digital Progress: Launch of HEM 2.0, upgraded package rates, and district-level implementation units.
Current Challenges
- Awareness & Utilisation Gap:
- Awareness remains low in some districts — e.g., a study showed only 8.9% urban and 18.8% rural awareness in certain areas.
- Supply-Side Constraints:
- Shortage of empanelled hospitals in rural/tribal areas; human resource gaps in public health facilities.
- Reimbursement Delays:(Haryana Case Study)
- Hospitals in Haryana report pending dues of ₹490 crore; payments often delayed, causing operational strain and service suspension by private hospitals.
- Fraud & Abuse Risks:
- Cases of inflated billing, false claims, and multiple beneficiary IDs linked to the same number flagged by CAG.
- Infrastructure Limitations:
- Existing facilities often lack advanced equipment, leading to referral overload on private hospitals.
Judicial / Policy Oversight and Government Initiatives
- CAG Audit Observations: Highlighted need for tighter fraud control and improved beneficiary database accuracy.
- Policy Steps: Expansion to new beneficiary categories, updated package rates, grievance redressal helplines, and real-time claim monitoring via IT dashboards.
Global Context and International Comparisons
- AB-PMJAY is among the largest health assurance schemes globally — comparable to national health systems in countries like the UK and Brazil in coverage, though still building infrastructure and service quality.
- Portability and digital integration are unique strengths compared to many developing country health schemes.
Conclusion and Way Forward
- AB-PMJAY has transformed India’s healthcare access landscape, but operational bottlenecks — especially reimbursement delays and uneven infrastructure — threaten its effectiveness.
- Way Forward:
- Streamline and time-bound claim settlement.
- Boost awareness campaigns through local health workers.
- Expand OPD, diagnostics, and medicine coverage to further cut OOPE.
- Strengthen rural health infrastructure and empanelment.
- Continue integration with digital health ecosystem for transparency and efficiency.
Previous Year Questions (PYQs)
- 2021: “Besides being a moral imperative of Welfare State, primary health structure is a necessary pre-condition for sustainable development.” Analyze. (10 Marks, 150 Words)
- “एक कल्याणकारी राज्य की नैतिक अनिवार्यता के अलावा, प्राथमिक स्वास्थ्य संरचना धारणीय विकास की एक आवश्यक पूर्व शर्त है।” विश्लेषण कीजिए।
- 2018: Appropriate local community-level healthcare intervention is a prerequisite to achieve ‘Health for All’ in India. Explain. (10 Marks, 150 Words)
- भारत में “सभी के लिए स्वास्थ्य” को प्राप्त करने के लिए समुचित स्थानीय सामुदायिक स्तरीय स्वास्थ्य देखभाल का मध्यक्षेप एक पूर्वपेक्षा है. व्याख्या कीजिए.
- 2016: “Professor Amartya Sen has advocated important reforms in the realms of primary education and primary health care. What are your suggestions to improve their status and performance?” (10 Marks, 150 Words)
- प्रोफेसर अमर्त्य सेन ने प्राथमिक शिक्षा तथा प्राथमिक स्वास्थ्य देखभाल के क्षेत्रों में महत्त्वपूर्ण सुधारों की वकालत की है। उनकी स्थिति और कार्य-निष्पादन में सुधार हेतु आपके क्या सुझाव हैं ?
- 2015: Public health system has limitation in providing universal health coverage. Do you think that private sector can help in bridging the gap? What other viable alternatives do you suggest? (12.5 Marks, 200 Words)
- सार्विक स्वास्थ्य संरक्षण प्रदान करने में सार्वजनिक स्वास्थ्य प्रणाली की अपनी परिसीमाएँ हैं। क्या आपके विचार में खाई को पाटने में निजी क्षेत्रक सहायक हो सकता है? आप अन्य कौन-से व्यवहार्य विकल्प सुझाएँगे?
UPSC Practice Questions
Prelims:
Q1. Which of the following are features of AB-PMJAY?
- Provides ₹5 lakh annual health cover per family.
- Coverage limited to below-poverty-line households as per 1991 census.
- Interstate portability for beneficiaries.
- Implemented by Ministry of Finance.
Options:
A) 1 and 3 only
B) 1, 2 and 3
C) 1 and 4 only
D) 1, 3 and 4
Answer: A) 1 and 3 only
Q2. The funding ratio under AB-PMJAY between Centre and State for Himalayan states is:
A) 60:40
B) 90:10
C) 75:25
D) 100:0
Answer: B) 90:10
Mains:
Ques: Critically analyse the achievements and challenges of AB-PMJAY in achieving Universal Health Coverage in India. Suggest reforms to improve its financial sustainability and service delivery. (10 Marks, 150 Words)
